Blood Clots After Flight
Long haul flying is a risk factor for vein blood clots. These include pulmonary embolism and deep vein thrombosis. This results in several challenges. First, how can we prevent blood clots after flight? and second, when can someone fly after suffering a blood clot?
Preventing Blood Clots After Flight
To prevent blood clots after flight, you need to know who is at risk. Some of the risks come from the flight, and some come from the passenger:
- Long flight – Flying more than 6 hours is considered a risk factor.
- Sitting in a window or middle seat.
- Not being able to get up during the flight. For instance, because of constant turbulence.
- A known tendency to clotting. For instance, a history of a previous blood clot after flying.
It is interesting, that even though there is not much data to suggest how to prevent blood clots after flight, the CDC has issued some guidance on the topic. Their recommendations make sense and include hydration, moving your legs while seated and getting up frequently to move around.
Medication to Prevent Blood Clots after Flight?
Some people will benefit from a low-dose blood thinner once before a long flight to prevent clots. Again, there are no real data to guide who to offer this to. But generally, if someone has proven that they are prone to clotting, then it may make sense. For instance, if thrombophilia testing has shown a significant clotting disorder, you would consider a low-dose blood thinner before major risks, and flying can be considered a relevant situation.
Examples of medications that might be relevant include a one time injection of enoxaparin 40 mg under the skin or taking 10 mg of rivaroxaban several hours prior to the flight.
Flying After a Clot
Deciding when to fly after having a clot is challenging. First, you want to avoid having more clots. But also, you need to know if flying is safe for you. Unfortunately, there is no hard data to guide these decisions. But here are a few questions you need to ask yourself:
- Are you still taking a blood thinner? If you are, then ironically you are still protected from more clots happening. This protection is not ironclad. But it is more than you would have if you were not taking the blood thinners.
- Are you using oxygen? Flying with oxygen can be complicated. Remember that there is less air pressure in the cabin than there is on the ground. So if you need oxygen on the ground, you will surely need it in the plane.
- Was your clot a deep vein thrombosis, a pulmonary embolism or both? Each condition has its own set of problems. For instance, flying after a DVT may worsen leg swelling. But flying after a PE can be more dangerous, especially if your breathing or heart have not normalized yet.
Flying after a Deep Vein Thrombosis
The problem with flying after a DVT is leg swelling. Basically, the relatively low cabin pressure induces leg swelling even in people with normal veins. So in some people, flying after a deep vein thrombosis will result in worse swelling. This is especially true if they suffer from post thrombotic syndrome.
Now, if you anticipate this, you can do something about it. The most obvious way to prevent leg swelling after flying is with compression stockings. The more severe your swelling, the tighter the compression stocking you might need.
Flying after a Pulmonary Embolism
There are two problems with flying after a pulmonary embolism. The first, is potential lack for oxygen. And the second, is a risk for worsening the function of the right ventricle of the heart. This is also tight to lack of oxygen. Basically, hypoxemia might elevate pulmonary arterial pressures, and if the right ventricle is not functioning normally, it may struggle against this elevated pressure.
Practically, we usually discuss flying after a PE clinically. In patients who did not have right heart strain as part of their PE, we usually do not order testing. If a patient can climb a couple of flights of stairs with a reasonable amount of effort, and if their oxygen levels remain normal, they are usually good to go. However, if there is a clinical problem, or if there is right heart strain, then we should discus testing.
Testing before Flying
The objective tool to check if your lungs are up for the task of flying is called the fit to fly test. Basically, you breath air that has less oxygen in it, while a machine tracks the oxygen in your blood. If you oxygen levels remain normal, then you are good to go.
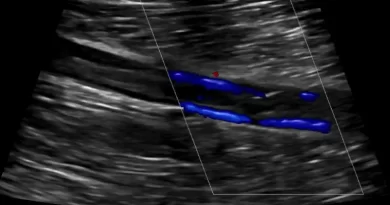
To test your heart function, the most simple test is a transthoracic echocardiogram (a “heart ultrasound”). This test can usually estimate the pulmonary arterial pressures. If an echocardiogram is not enough, you may opt for a right heart catheterization.




Pingback: One Swollen Leg: 10 Causes and How to Diagnose Them
Pingback: How Long to Anticoagulate a Blood Clot? Many Factors to Consider