Cancer and Blood Clots
It is well known that there is an association of cancer and blood clots. Patients with certain types of cancer are at a high risk for pulmonary embolism, deep vein thrombosis and even arterial clots. But not all cancer types are associated with clotting. Still, there are implications for diagnosis and treatment.
The Association of Cancer and Blood Clots
Jean-Baptiste Bouillaud described the association of cancer and blood clots back in 1823. But actually Armand Trousseau who again described this association in 1865 got all the fame.
Indeed, clotting risk increases in many types of cancer. But not all cancers are made the same. Most risk is with pancreas, brain, lung, and ovarian cancers. Low risk is with breast or prostate cancer. But these cancers are prevalent. So seeing blood clots in a patient with either breast or prostate cancer is not uncommon. Also, cancer stage is relevant. More advanced cancer is more likely to cause clots. The RIETE registry have an interesting online tool that can help visualize some of the vital statistics of cancer and blood clots.
A cancer will show up in 20-30% of patients who suffer a first unprovoked venous clot. Indeed, the relative-risk of clots in cancer patients (compared to non-cancer patients) is high. But a patient will want to know their actual risk, not their relative risk. Again, there is variability in the data. And again, not all cancers and not all patients are the same. But a typical range is 0.5-2% of all cancer patients will have a blood clot.
Mechanism for Blood Clots in Cancer Patients
There is more than one mechanism for blood clots in cancer patients. The cancer, the treatment and the patient all contribute to the risk for clots. Some of these risk factors are more obvious than others. For instance, why is the patient a risk for clotting? Well, the reason the patient is a risk factor, is because cancer patients may be immobile. Immobility is a known risk factor for clotting. Also, many patients will need procedures. Blood clots after surgery are common.
It might also not be obvious why cancer treatment is a risk for thrombosis. But if you think of treatment in the broad sense of the word, the connection becomes obvious. This is because treatment includes intravenous catheters and surgery. Obviously, both are risks for clots. Treatment also includes hormonal therapy. We know that estrogen and estrogen analogues in particular are risk factors for clotting. Still, the full picture is more complicated because many other forms of cancer treatments can also be the cause for clotting.
Finally, the tumor itself. Obviously, this is the main risk for thrombosis. Actually, tumors cause clots by a variety of mechanisms. These include effects on the endothelium, platelets, inflammatory system and more.
Will All Cancer Patients Develop Clots?
The short answer is, of course not. First, not all cancer types are the same. Second, cancer extent matters. For instance, metastatic cancer is different than low-grade localized disease. But how can you remember all cancer types and their association with clotting? That is impossible, of course, But still, there are some cancer-types that are more common. There are a few scoring systems that help us calculate clotting risk in those types of malignancy. A useful tool is the Khorana risk score (based on a 2008 paper). There are other similar risk scores (see Table 2 in this publication).
Why does this matter? In practice, we will treat those patients who develop patients, correct? Well, of course that is correct. But there are also implications for prophylaxis. Two studies, one with apixaban and one with rivaroxaban have shown limited benefit. But bleeding was an issue. So we might be best off offering prophylaxis with apixaban 2.5 mg BID or rivaroxaban 10 mg QD to cancer patients with high-risk scores. We probably need to exclude patients without high-risk for bleeding characteristics such as previous bleeding, dual anti-platelet agent therapy etc.
Diagnosis
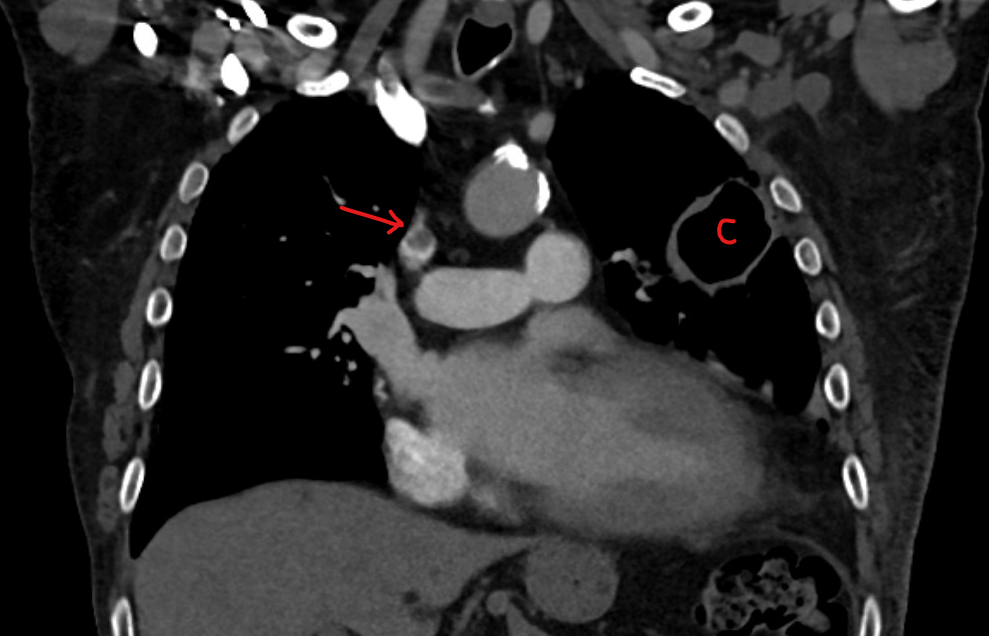
The diagnosis of venous and arterial thrombosis in cancer patients is similar to any other patient. Perhaps one difference is that cancer patients tend to have imaging studies for the cancer. So sometimes clots are discovered incidentally. A common example is an incidental findings of a pulmonary embolism on a staging chest CT.
Symptoms are also similar to non-cancer patients. Leg pain and swelling are typical for deep vein thrombosis. In fact, cancer leg pain is an unfortunately common symptom. Chest pain and shortness of breath are typical of pulmonary embolism. Arterial clots will present with blocked flow to a vital organ. For instance, as a cold limb.
Ultrasound is the most common test to use to visualize and prove a deep vein thrombosis. CT of the chest is the most common scan to prove a pulmonary embolism. A V/Q scan is also possible.
Screening for Cancer
Should patients who have an otherwise unprovoked venous thromboembolic event undergo screening for cancer? Two large trials examined this issue. Both had results that did not support this practice. However, there is logic to say that patients who are otherwise at higher risk for malignancy may deserve screening.
The RIETE network are running two trials: SOME-RIETE and VaLRIETEs to examine this hypothesis. They will try to answer whether 18F-FDG PET/CT will be beneficial for patients after unprovoked VTE. These studies will validate and utilize the RIETE score. Notably, the RIETE score is not the only score out there trying to predict the likelihood of cancer post VTE.
Treatment Implications
If a venous clot happens in a cancer patient, there are typically four implications:
- Treatment choice
- Duration of therapy
- Balancing re-thrombosis and bleeding risk
- Managing the need for anticoagulation interruptions
Anticoagulation Choice for Cancer Associated Thrombosis
In the past, we had only two medications to choose from: Warfarin and low-molecular weight heparin. Between those two, we used to choose the heparin. This was an unfortunate choice for patients because it meant they had to suffer through injections, for at least 6 months.
However, since then there has been progress. Now we can offer cancer patients rivaroxaban or apixaban. We consider both non-inferior to low-molecular weight heparin. In 2023, the final results of the CANVAS trial confirmed that yet again. The American Society of Hematology now recommends the use of these agents for cancer associated blood clots alongside low-molecular weight heparin. The Chest College of Physicians guidelines from 2021 actually placed these medications above low-molecular weight heparin for this purpose.
A question that often comes up is whether we should decrease the dose in cancer patients after 6 months of treatment as we do in non-cancer patients. I found one abstract that examined this. According to their data, lowering the dose made sense because it resulted in a minor increase in clots, but a substantial decrease in bleeding.
There is one important caveat. Both these medications can cause an excess of GI bleeds. So we should avoid them in patients with GI malignancy or with a risk for GI bleeding.
Treatment Duration for Cancer Associated Blood Clots?
As we all know, treatment duration is dictated by recurrence risk. In other words, if recurrence risk is low, then we treat for a short duration. But if recurrence risk is high, we treat for a longer duration. The recurrence risk for venous thrombosis in cancer is very high. So, treatment should be longer.
It is customary to say that treatment should not stop before the cancer has been cured for at least 6 months. Of course, this decision has to take into account other factors, and especially bleeding risk.
In the past, we used to treat blood clots in cancer patients with injectable blood thinners called low molecular weight heparin. However, more recent information taught us that other medications such as rivaroxaban (Xarelto) and apixaban (Eliquis) are as effective in cancer patients. Patients can take these medications as pills. So injections are no longer necessary.
A study was published in the New England Journal of Medicine in March of 2025. It showed that if you need to treat a blood clot in a cancer patient for longer than 3-6 months, then you can reduce the dose of the medication. Reducing the dose did not result in more recurrence of clots, but reduced risk of bleeding.
Prophylaxis?
It is important to differentiate between treatment and prevention. Rivaroxaban was not effective in preventing venous thrombosis in ambulatory cancer patients. On the other hand, apixaban was effective.
Cancer and Bleeding
It is known that cancer patients have an increased risk for bleeding. This has particular implications if they suffer a blood clot. Obviously, treatment needs to balance the risk for bleeding with the need to treat the clot.
Anticoagulation Interruptions
Unfortunately, there are several reasons to interrupt anticoagulation in cancer patients. First, procedures. A patient with cancer might need special lines inserted, or major surgery related to the cancer. Managing surgery and blood thinners can be complicated. But also the cancer or the treatment might affect blood counts. If the platelet count goes down or if the hematocrit drops, we sometimes have to stop anticoagulation.