Chronic Mesenteric Ischemia
When not enough blood is reaching the intestines, that will lead to symptoms of chronic mesenteric ischemia. Symptoms usually develop over time. Chronic mesenteric ischemia is different from acute mesenteric ischemia.
Causes
The most common cause is atherosclerosis. Usually both the celiac artery and the superior mesenteric artery will have severe stenosis. There is debate about whether one diseased artery can cause symptoms. But remember, that most patients with mesenteric artery stenosis will not have any symptoms of mesenteric ischemia. This is because of ample collateral flow and redundancy in the system.
A different entity is non obstructive mesenteric ischemia (NOMI). It is basically a condition of low flow because of cardiac or pulmonary disease. Non-occlusive mesenteric ischemia is more a cause of acute mesenteric ischemia than of chronic symptoms.
Chronic Mesenteric Ischemia Symptoms
Patients will describe pain with food. The pain will be severe, epigastric, gnawing in quality and start about 30 minutes after eating. Many patients will report pain even with small amounts of food. The pain is often so severe that patients are afraid to eat. This “classic” description is quite true in real life. Patients definitely lose large amounts of weight as a result of their fear of eating.
Symptoms of chronic mesenteric ischemia do not include diarrhea or constipation. There is debate about whether nausea and belching can be part of this syndrome. There is also a possibility of gastric ischemia from severe celiac artery stenosis. But this is not common.
Diagnosis
We suspect the diagnosis when a patient complains of severe abdominal pain and weight loss. Then, on exam we can often hear an epigastric bruit. But, once you suspect the diagnosis, you need to obtain imaging to prove it. Maybe surprisingly, lactate is not part of the evaluation. The lactate can be normal in people with true disease. Obviously, thrombophilia testing is also not part of the diagnosis.
Usually, we start with a mesenteric artery ultrasound. On the one hand an ultrasound is safe and cheap. It also is sensitive at detecting elevated flow velocities in the arteries:
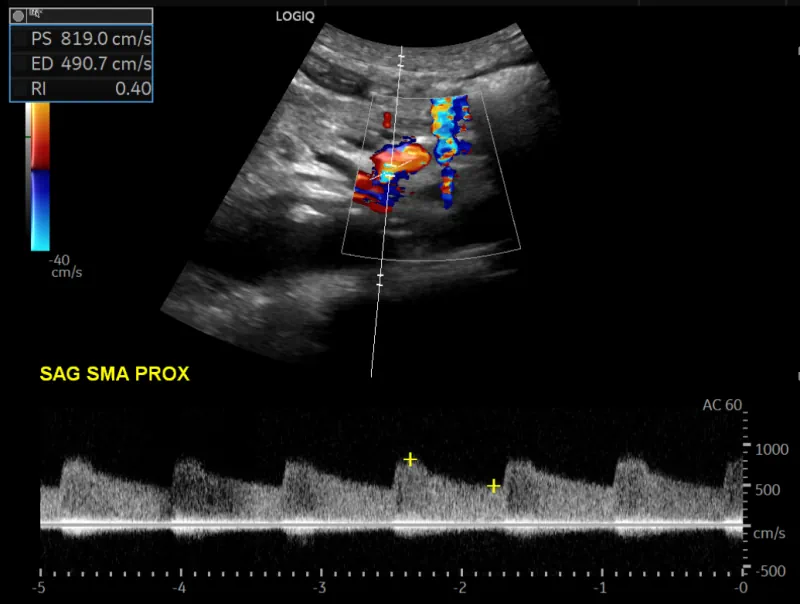
But it has two important disadvantages. First, image quality. You often cannot see the mesenteric arteries properly, either because of overlying bowel gas or just because. The second problem is clinical correlation. It is not uncommon for the velocity to be elevated, but in the end the patient does not really have stenosis.
So, usually, you will need another test. That will either be a CT or an MRI.
Of course, another option is to go straight to an angiogram. The obvious advantage of an angiogram is that you can both make the diagnosis and treat. A second advantage is the ability to measure pressures across a lesion. So you can prove that a stenosis is hemodynamically significant. An angiogram also allows to image collaterals and assess overall flow in a dynamic way that a CT or MRI cannot. But there are two disadvantages. First, it requires contrast. That will not be appropriate in all patients. And second, it is an invasive procedure that is not devoid of complications.
Other Tests
The European guidelines for chronic mesenteric ischemia suggest that some patients will need more testing. First, they suggest endoscopy. The idea here is to rule out alternative diagnoses. Second, they suggest that some patients will require functional testing to prove the diagnosis. I have not seen these used, so I do not have a clinical sense for the utility of these tests.
Chronic Mesenteric Ischemia Treatment
The treatment of chronic mesenteric ischemia has two components. The first, is medical. Patients who have severe mesenteric artery stenosis will often have diffuse system atherosclerosis. So risk-factor modification is logical. Most patients will need an antiplatelet agent such as aspirin and a high-intensity statin.
The second component of treatment is intervention. This is usually done with endovascular tools. But surgical bypass is a possibility.
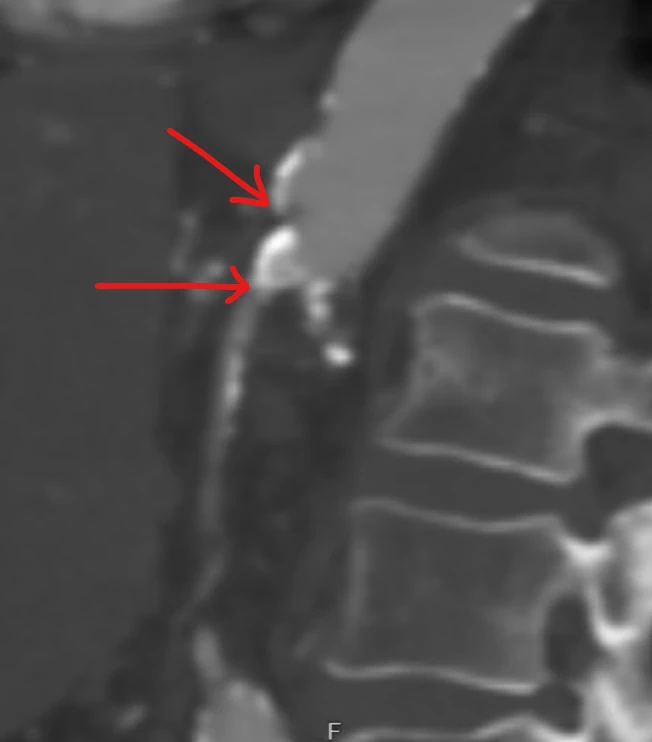
Median Arcuate Ligament Syndrome
Median arcuate ligament syndrome (MALS) is when the diaphragm pinches the celiac artery and the surrounding celiac plexus. This pinch causes a characteristic kink in the artery. Seeing this on a CT scan is actually not uncommon. But sometimes the pinch will be associated with symptoms that are hard to distinguish from those of chronic mesenteric ischemia. Knowing when MALS is “real” and when it is only an imaging finding can be challenging.

