Paget Schroetter Syndrome
Sometimes a compression of a vein causes a deep vein thrombosis. The mechanism is by preventing normal blood flow. Stagnant blood tends to clot. We have written about such a compression in the pelvic veins. That is called May-Thurner syndrome or Iliac Vein Compression Syndrome. When the compression occurs in the upper chest then a clot will develop in the subclavian and axillary veins. This is known as Paget Schroetter Syndrome. It is also known as venous thoracic outlet syndrome.
Symptoms of Paget Schroetter Syndrome
Some people will complain of arm swelling with activity long before they experience a deep vein thrombosis. Classically, overhead activities precipitate the problem. These include repetitive throwing of a ball (such as with baseball pitchers), swimming (typically freestyle) and shoveling (such as snow). We have seen clots develop in persons who performed excessive push-ups.
Sometimes the clot does not form, but the vein scars over time. When this happens, typically there will be multiple visible veins around the chest. These serve as natural bypasses to overcome the pinching of the main venous channel. These veins are called sentinel veins or Urschel veins (named after a physician who published extensively on this topic).
Diagnosis
The easiest way to make the diagnosis is if a patient presents with an acute clot in their subclavian vein that was precipitated by a typical activity. But sometimes the diagnosis is not so clear cut. For instance, cancer patients my experience clots in unusual locations, including in the upper extremities.
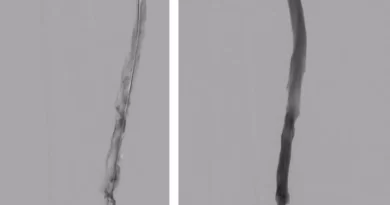
Other than clinical presentation, the classic imaging study to make the diagnosis is an ultrasound examination. The ultrasound will show the extensive clot. But once we start treatment with anticoagulation, we usually aim to follow with invasive therapy. This includes thrombolysis of the blocked vein. Then, we can supplement the diagnosis with provocative maneuvers under angio, to look for venous compression.
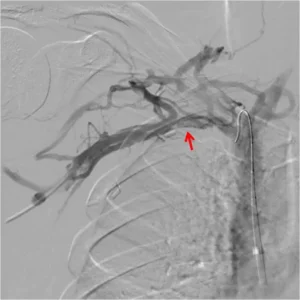
A clinical challenge occurs if we find vein compression on the contralateral side to the clot. The question then is whether we need to treat that side as well.
Treatment
As noted, we start with anticoagulation. Then, we often supplement with catheter directed thrombolysis, usually during the index admission. If we find a cervical rib as the cause of the compression, we usually recommend prompt rib resection or resection of a costoclavicular ligament. If the patient is a very active person such as a professional athlete, we may recommend bilateral cervical rib resections, to prevent clos from happening on the other side and to allow full return to activity.
Once the anatomical lesion is fixed, it is important to discuss duration of anticoagulation. Many will say that if you remove the cause of the venous pinch, a patient can receive a blood thinner for a limited amount of time, such as for 3 months after the surgery.