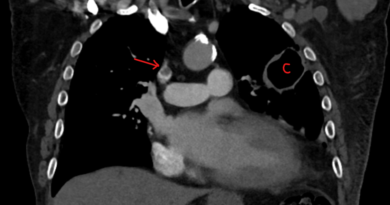
Systemic Thrombolysis for Pulmonary Embolism
Systemic thrombolysis for pulmonary embolism has been around since the 1960’s. It is true that modern PE treatment includes more targeted procedures including catheter directed thrombolysis and mechanical thrombectomy. But there is still a role for systemic thrombolysis.
How does Thrombolysis Work?
Different from anticoagulation, thrombolysis actually dissolves clots. They do so by converting plasminogen to plasmin. Then, plasmin breaks down fibrin which leads to clot lysis.
Importantly, if plasminogen is converted to plasmin systemically, it will promote a systemic coagulopathy.
Thrombolytic Agents
The three approved agents are streptokinase, urokinase and recombinant tissue plasminogen activator (rt-PA). Another name for rt-PA is alteplase.
Tillet discovered streptokinase in 1933 when he observed the hemolytic effect of certain beta-hemolytic streptococci. An interesting fact about urokinase is that it is produced from human urine or from renal embryonic cells. The thrombolytic effect of human urine was published in Nature in 1947, and I really don’t know who the authors thought to check that…
Potential Advantages of Systemic Thrombolysis for Pulmonary Embolism
The backbone of pulmonary embolism treatment is anticoagulation. But anticoagulation dose not actually dissolve clots. And thrombolytics do. So they may have several advantages:
- More rapid clot lysis and thus faster clinical improvement
- Reduce the incidence of recurrent pulmonary embolism (by dissolving clots that could potentially dislodge to the lungs – especially deep vein thrombosis)
- Prevent the development of chronic thromboembolic pulmonary hypertension
But have any of these possible advantages actually pan out? For most patients with pulmonary embolism, the short answer is “no“. Even with perfusion scans that track how clot is cleared from the lungs there is a quick catch-up with anticoagulation within a few days.
So where does systemic thrombolysis for pulmonary embolism really have an advantage? Likely, mainly for patients who are very sick. These are going to be patients with high-risk PE and especially if they are unstable. Systemic thrombolysis will have the most advantage in centers that do not have advanced therapies. Because in more advanced centers, there are other possibilities to stabilize patients. For instance with ECMO.
Complications of Systemic Thrombolysis for Pulmonary Embolism
The main complication of thrombolytic therapy is bleeding. Depending on the definition, the rate of major bleeding with this treatment is around 10%. The rate of intracranial hemorrhage is around the 1-1.5%. About half the patients who suffer an intracranial hemorrhage will die. Many others will remain limited.
We can try to minimize the risk of bleeding by avoiding procedures during the thrombolysis infusion. This should include phlebotomy and arterial punctures.
Other complications exist. Most important complications include allergic reactions and hypotension. In this context we need to mention streptokinase. This agent triggers an immune response. So we need to avoid it in patients who received it within 6 months. It is also specifically implicated in hypotension.
How to Administer Systemic Thrombolysis for Pulmonary Embolism
First, we need to remember that the original studies of these medicines excluded patients with clots older than 5 days. Later, they expanded the use to 14 days. But they observed a much lower lytic effect as time progressed.
Once we decided to administer one of these agents, we should do so quickly. Each thrombolytic agent has a specific dose an infusion time. The most common agent to administer is rt-PA. It has the fastest effect:
| Drug | Regimen |
| Streptokinase | 250,000 Units over 30 minutes, followed by 100,000 units/hour for 24 hours |
| Urokinase | 4,400 units/Kg over 10 minutes, followed by 4,400 units/Kg/hour for 12-24 hours |
| rt-PA | 100 mg over 2 hours |
A common question is whether to administer a bolus. It seems that there is no real advantage for a bolus and so it is usually avoided.
Another question that often comes up is whether to stop the heparin infusion. Different than in the treatment of myocardial infarction, in pulmonary embolism treatment we stop the heparin infusion while administering the systemic thrombolytic agent. By the way, this is also different than when we administer catheter directed thrombolysis.
Contraindications for Thrombolysis
The contraindications that we usually quote for thrombolysis were first published in 1980. They were a product of a National Institute of Health workgroup. Practically, we extrapolate these recommended contraindications to pulmonary embolism treatment. There are few absolute contraindications:
- Active internal bleeding
- Recent stroke or other intracranial process (within 2 months)
And then there are several major relative contraindications:
- Recent major surgery (within 10 days) or major trauma
- A GI bleed that occurred recently
- Hypertension above 200/110 mmHg
Finally, there are several minor relative contraindications:
- Minor trauma (including CPR)
- Bacterial endocarditis
- High likelihood of left heart thrombus (e.g., atrial fibrillation)
- Coagulopathy (e.g., severe liver or renal disease)
- Pregnancy
- Age over 75 years
- Diabetic hemorrhagic retinopathy