Anticoagulation Failure
Anticoagulation works in most people. In fact, the rate of anticoagulation failure is quite low. For this reason, if a patient experiences worsening clot despite anticoagulation, we must always try to understand the cause.
What is Anticoagulation Failure?
A person who has a deep vein thrombosis or a pulmonary embolism and who is taking their blood thinners, should usually improve over time. Unfortunately, not everyone improves. Of course, this does not automatically mean that there is a problem with treatment. Some people might develop post-thrombotic syndrome after deep vein thrombosis. Others might develop chronic thromboembolic pulmonary hypertension after pulmonary embolism.
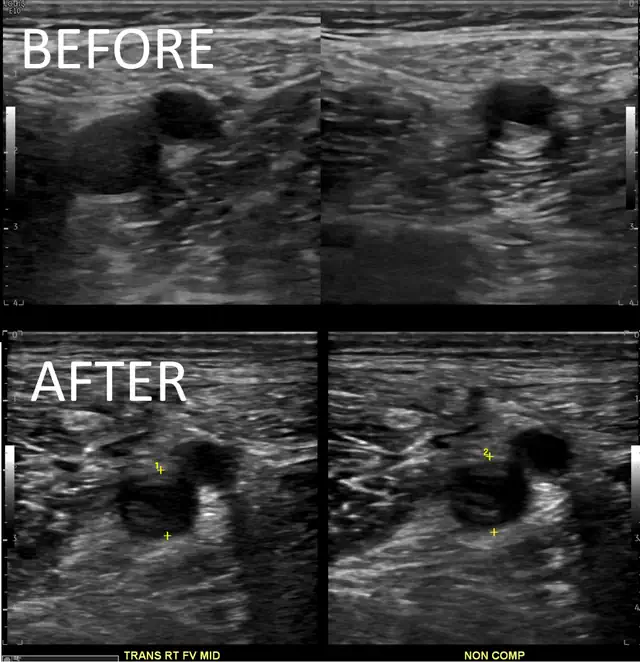
It is important to know that it can be hard to know if a person has acute or chronic clot. But in some people we can prove that there is more new clot. For instance, the DVT extended compared to a previous ultrasound. Or, there are new PE in a location where there were none before. If that happens, we call it anticoagulation failure.
Potential Causes
Because anticoagulation failure is so uncommon, there are very few things we should think about if it happens.
A Leading Cause for Anticoagulation Failure is Non-Compliance
First, consider non-compliance. This basically means that the patient may not have taken the blood thinners the way they were supposed to. Everybody forgets to take their pills from time to time. But the longer a person neglects to take their blood thinners, the higher the chance of recurrent clot.
External or Man-made Risk Factors
Next, we need to think about external risk-factors. We know that acute illness can increase the risk for clotting. So if a person who has been doing fine with their blood thinners is suddenly injured or sick, that may put them at risk for more clots. Specifically, COVID-19 blood clots are a hotly contested issue. Venous thrombosis and immobility are tied together as well. So if a person is chronically immobile, that might contribute to their risk of further clotting.
Another possible risk-factor is an IVC filter. We know that more DVT happen when IVC filters are in place. This happens with or without anticoagulation. Also, an IVC filter can cause complications including IVC thrombosis. Finally, IVC filters are not perfect. A person might have a PE despite an IVC filter.
Cancer and Blood Clots
Unfortunately, we must also think about cancer. Unfortunately, cancer and blood clots often go hand in hand. So, if a patient is doing everything they are supposed to be doing, and still have worse or new clots, think about cancer.
Genetic and Blood Disorders and Anticoagulation Failure
Some people have genetic disorders that make them more prone to clotting. Usually, testing for these disorders is not very useful. But, if anticoagulation failure happens, thrombophilia testing may be useful. One specific disorder to think about is the antiphospholipid antibody syndrome. People who have this condition should be very careful about taking their blood thinners. Also, they should take Warfarin or injectable agents, and not one of the direct oral anticoagulants. So apixaban (Eliquis) and rivaroxaban (Xarelto) are not the best medications for these people.
Vein Compression
Finally, some people will have an anatomical reason for anticoagulation failure. The most common will be May Thurner syndrome. In this condition the right iliac artery compresses the left iliac vein. The compression is chronic, but at some point a clot can happen. If this is a central reason for the clot, anticoagulation will typically not be enough. Also, we need to remember that there are other causes for compression. For instance pelvic tumors.
Management
The management of anticoagulation failure depends on the cause. Sometimes, the solution is easy. Just remove the risk-factor. For instance, help a person to remember to take their medication or help them be more mobile. If a patient has antiphospholipid antibody syndrome, switching to an appropriate blood thinner at the correct dose is the best solution. But sometimes solutions need to be more creative. We may offer a person a higher dose of the same blood thinner. Or, we may offer a different blood thinner, hoping that the different mechanism will have a better effect.
Final word – We wrote another article on clotting despite anticoagulation. Reading both articles may be complementary.


Pingback: May Thurner Syndrome: Symptoms, Diagnosis and Treatment
Pingback: Pulmonary Embolism Response Team